Efficacy of Face Masks against COVID-19
This project aims to close the evidence gap by investigating the effectiveness of face masks to reduce exposure to respiratory droplets/aerosols containing the COVID-19 virus. We propose to use detailed coupled flow and solid/cloth mechanics modelling to this end. Once barrier effectiveness is understood, improvements to face masks can be identified using the modelling at the filter-fibre scale approach outlined below. The findings will enable us to make recommendations on how face mask design can be improved with the aim to reduce COVID-19 infection rates in NHS and key workers and the public.
Background: Since the global outbreak of pandemic coronavirus (COVID-19), wearing surgical face masks has become increasingly common amongst healthcare providers and the general public. These are loose-fitting disposable face masks covering the wearer’s nose and mouth. We plan to investigate the effectiveness of surgical masks in protecting the wearer from COVID-19 as well as protecting others where the wearer has the virus. Surgical masks are intended to act as a barrier from the wearer to others. There is an ongoing debate about the use of face masks in the community as the evidence to support their use in the community has been limited up until now. It’s no wonder then that many people are still confused about the efficacy of masks in preventing the spread of COVID-19.
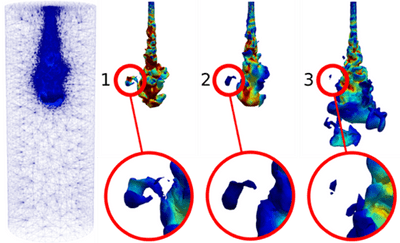
This project will use detailed coupled flow and solid/cloth mechanics modelling to investigate the effectiveness of face masks to prevent virus-laden droplet/particle transmission from infected individuals. It aims to close that evidence gap and investigate exposure hazards to COVID-19 with and without face masks. It will eventually (outside the scope of this initial proposal) analyse the face and the cloth movement of an individual with the resulting flows while breathing. This is very important, for example, in seal assessment in loose-fitting masks as commonly used by the general public. It will also look at the detailed droplet laden flows through the porous media of face masks using both analytical (e.g. bundle of tubes) and numerical treatments (the solid-fluid modelling central to this proposal). This will enable us to answer questions like,
1, Is viral transport through face masks facilitated (a) by wetted ‘pores’ between fibres, in which case we need to understand how water invades and provides bridging pathways from one side to the other, or (b) by direct transport on dust particles if they are small enough to pass through pores? 2) Does Virus interact with solid surfaces (adsorption) as it passes through wetted pores? 3) Is there a way to develop a cheap treatment that makes masks hydrophobic and thus permeable to gas but impermeable to virus-laden water droplets? 4) Could modelling of drying and treatments of used masks be recommended for testing so masks can be re-used?
